Toxic or drug-induced hepatitis
Toxic hepatitis is inflammation of the liver caused by exposure to toxins. Common triggers include:
Alcohol
Chemicals
Certain medicines
Nutritional supplements
The onset of toxic hepatitis can vary:
Sometimes symptoms appear within hours or days of exposure to a toxin.
In other cases, symptoms may develop after months of regular exposure.
Symptoms often improve once exposure to the toxin stops. However, toxic hepatitis can sometimes cause permanent liver damage, including:
Scarring of liver tissue (cirrhosis)
Liver failure, which can be life-threatening
Symptoms
Mild toxic hepatitis might not cause symptoms. It might be found with blood tests. When symptoms of toxic hepatitis occur, they can include:
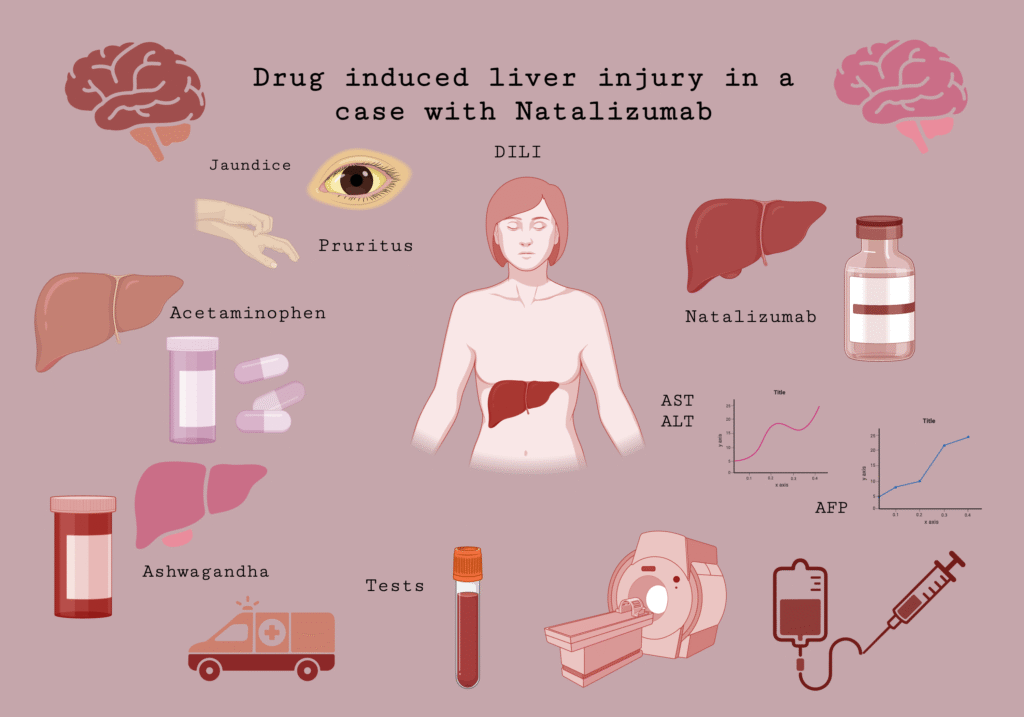
- Yellowing of the skin, which may be easier to see on white skin. Yellowing of the whites of the eyes. This yellowing is called jaundice.
- Itching.
- Pain in the upper right part of the stomach area.
- Fatigue.
- Loss of appetite.
- Nausea and vomiting.
- Rash.
- Fever.
- Weight loss.
- Dark or tea-colored urine.
When to see a doctor
See a healthcare professional right away if you have symptoms that worry you.
Taking too much of some medicines, such as acetaminophen (Tylenol, others), may lead to liver failure. Get medical care right away for an adult or a child who has taken too much acetaminophen. Symptoms of a possible acetaminophen overdose include:
- Loss of appetite.
- Nausea and vomiting.
- Pain in the upper stomach area.
- Coma.
If you suspect an acetaminophen overdose, immediately call 911 or your local emergency services. In the United States, call a poison control center at 800-222-1222. Do not wait to see symptoms. An acetaminophen overdose can be fatal. But it can be treated soon after the acetaminophen is taken.
What does your liver do?
Your liver is one of your largest organs. It helps clean (filter) your blood and remove toxins from your body.
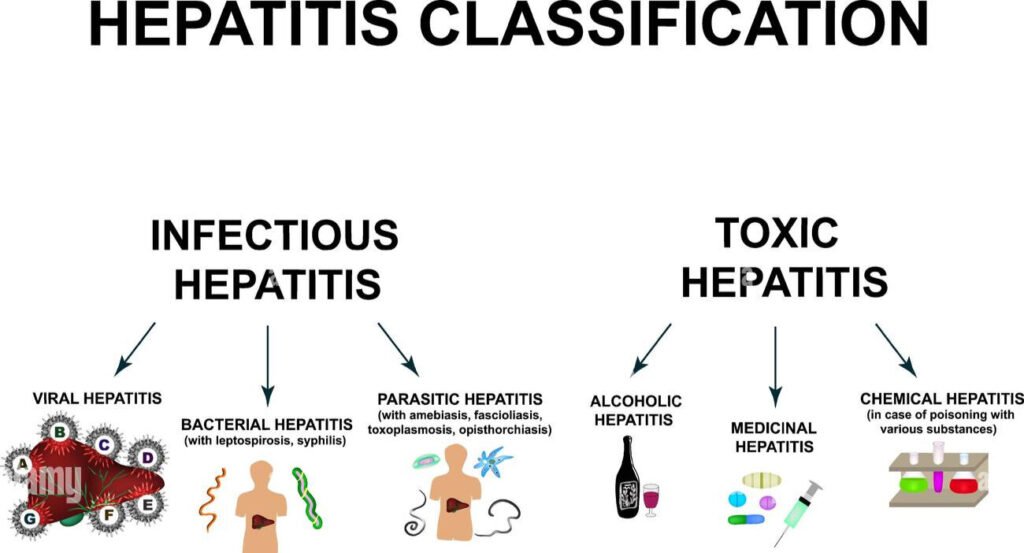
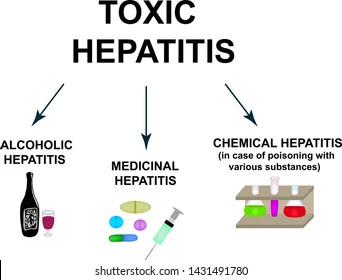
Are there different types of toxic hepatitis?
Types of toxic hepatitis include:
- Acute toxic hepatitis: This type develops suddenly. Symptoms occur immediately or shortly after exposure to a toxic substance.
- Chronic toxic hepatitis: This type may take longer to develop. You may not have any hepatitis symptoms for weeks or months.
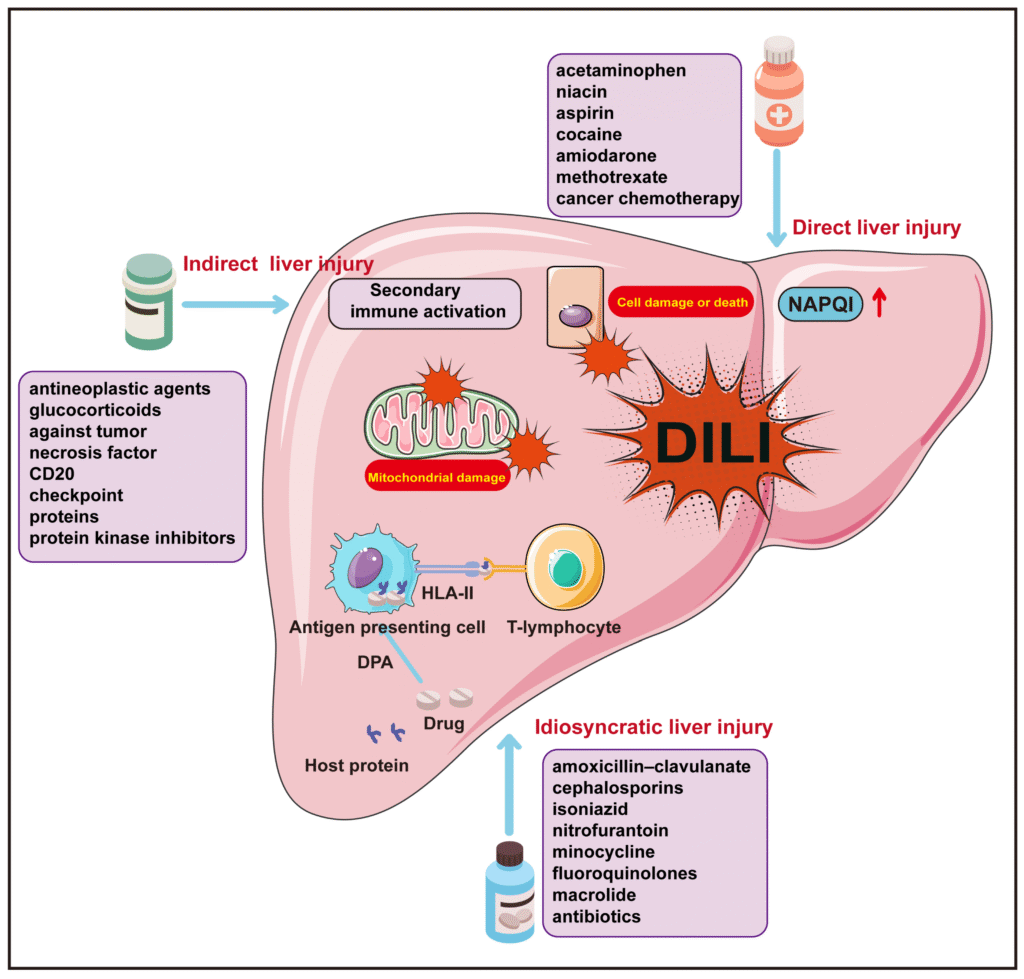
Healthcare providers also categorize types of hepatitis according to the cause:
- Chemical-induced hepatitis: You develop this because of exposure to chemicals through ingesting, breathing or touching the chemical.
- Drug-induced hepatitis: You develop this type because of taking too much of certain medications, such as acetaminophen, nonsteroidal anti-inflammatory drugs and other drugs.
- Alcohol-induced hepatitis: This type is due to alcohol use disorder, especially if you also use recreational drugs.
What causes toxic hepatitis?
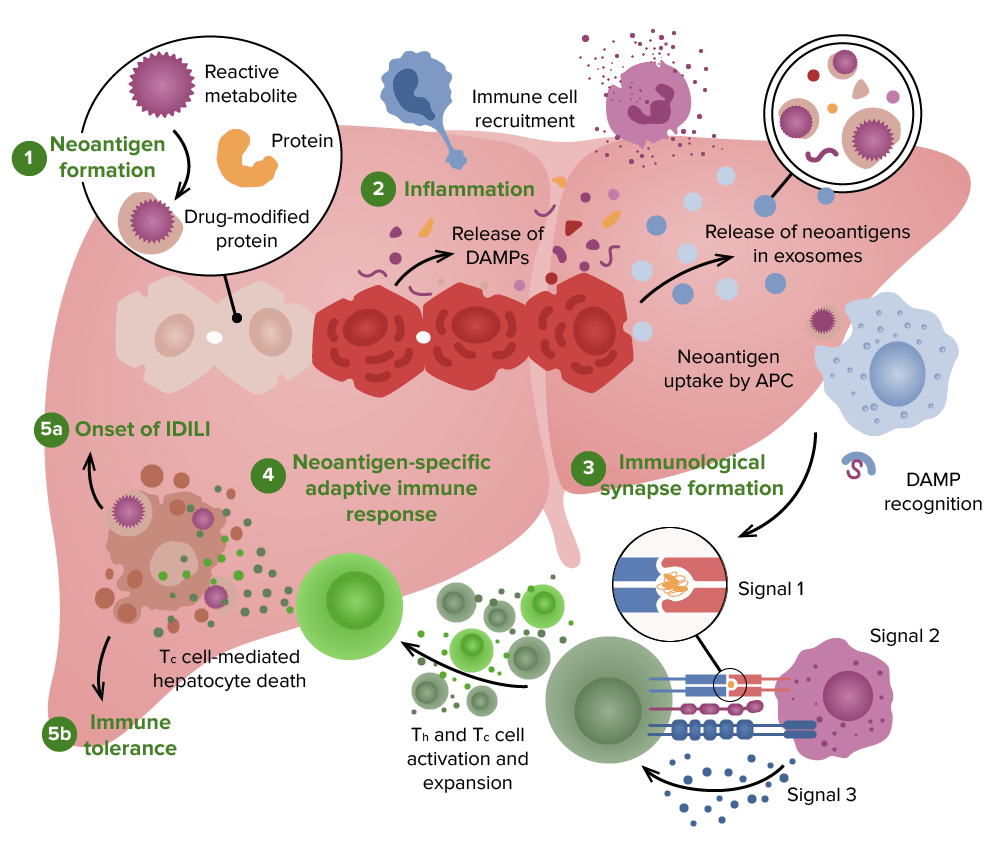
Toxic hepatitis occurs when the liver becomes inflamed due to exposure to harmful substances. Not everyone exposed to these substances will develop toxic hepatitis—reactions can vary from person to person.
Symptoms may appear soon after exposure or may take weeks to months to develop.
Common causes include:
Medications (such as acetaminophen or certain antibiotics)
Alcohol
Industrial or household chemicals
Herbal or nutritional supplements
Drug-induced hepatotoxicity
This type of toxic hepatitis results from medications or supplements. Certain medications or dietary supplements may cause this drug-induced liver injury, including:
- Herbal supplements.
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Prescription medications.
Alcohol-induced toxic hepatitis
Drinking too much alcohol can cause alcohol-induced hepatitis. If you experience alcohol use disorder, it’s important to talk to a healthcare provider.
Acetaminophen liver toxicity
You may develop liver toxicity if you take too much acetaminophen (Tylenol®), an over-the-counter pain reliever. Many people use acetaminophen to treat fever and pain. Most adults shouldn’t take:
- More than 4,000 milligrams of acetaminophen in one day (24 hours).
- Acetaminophen for more than 10 days in a row.
Too much acetaminophen can be dangerous if you already have liver disease. Call your healthcare provider right away if you take more than the recommended dose. Your provider may order an acetaminophen level test.
Vitamin A liver toxicity
Taking too much vitamin A (more than 40,000 IU daily) can cause vitamin A liver toxicity. Talk to your healthcare provider about any supplements or over-the-counter medications you take.
Diagnosis and Tests
How do healthcare providers diagnose toxic hepatitis?
Your healthcare provider talks with you about your symptoms and lifestyle. They also do a physical examination. Your provider may order tests to confirm a toxic hepatitis diagnosis.
What toxic hepatitis blood tests will I have?
You may have certain blood tests such as:
- Comprehensive metabolic panel (CMP).
- Liver function tests.
Your provider may order a blood alcohol content (BAC) or drug test. Blood and urine tests help your provider figure out the level of alcohol or drugs in your blood.
Are there other tests for toxic hepatitis?
If your provider wants more information about your liver health, you may have:
- Imaging tests, such as CT scan or MRI.
- Liver biopsy.
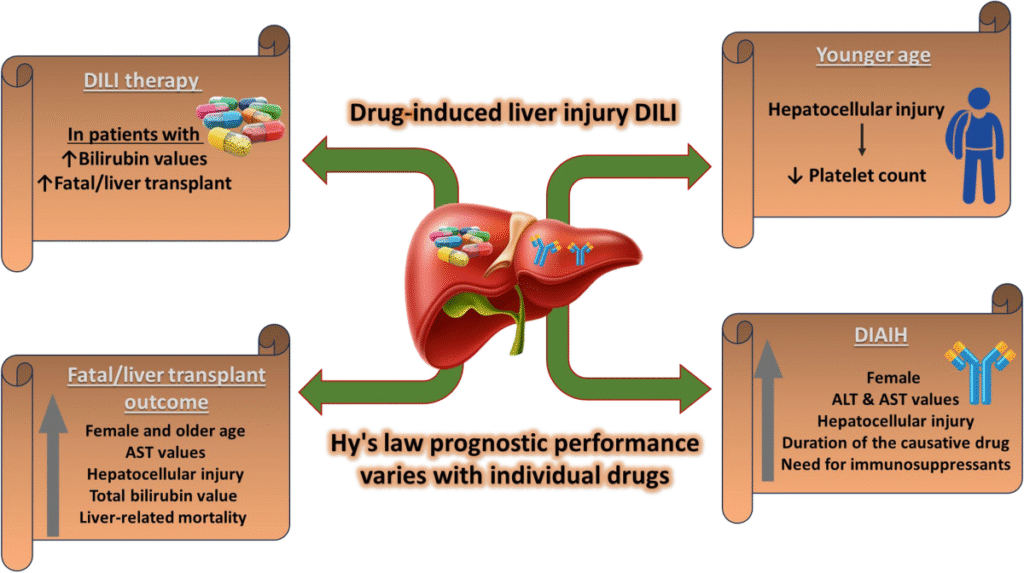
Management and Treatment
Treatment for toxic hepatitis depends on how much the liver is affected. Your healthcare provider may recommend:
Avoiding medications or supplements that can harm the liver
Stopping alcohol consumption
Changing workplace duties if you’re exposed to harmful chemicals
Using protective equipment when working with certain chemicals
Is Toxic Hepatitis Curable?
In many cases, toxic hepatitis is curable. The liver can regenerate and replace damaged cells over time, reversing much of the harm. However, if liver disease has progressed to cirrhosis, there is a risk of liver failure, and your care team may discuss the possibility of a liver transplant.
Recovery Time
Recovery from toxic hepatitis depends on:
How long the condition has been present
The extent of liver damage
If the liver damage is mild to moderate, healing may take a few weeks to months as the liver regenerates healthy cells.