Metabolic dysfunction-associated steatotic liver disease (MASLD)
Metabolic dysfunction-associated steatotic liver disease (MASLD) is a chronic liver condition that develops when too much fat builds up in the liver. It is strongly linked to being overweight or obese and is often associated with other health problems such as type 2 diabetes, heart disease, and circulatory disorders.
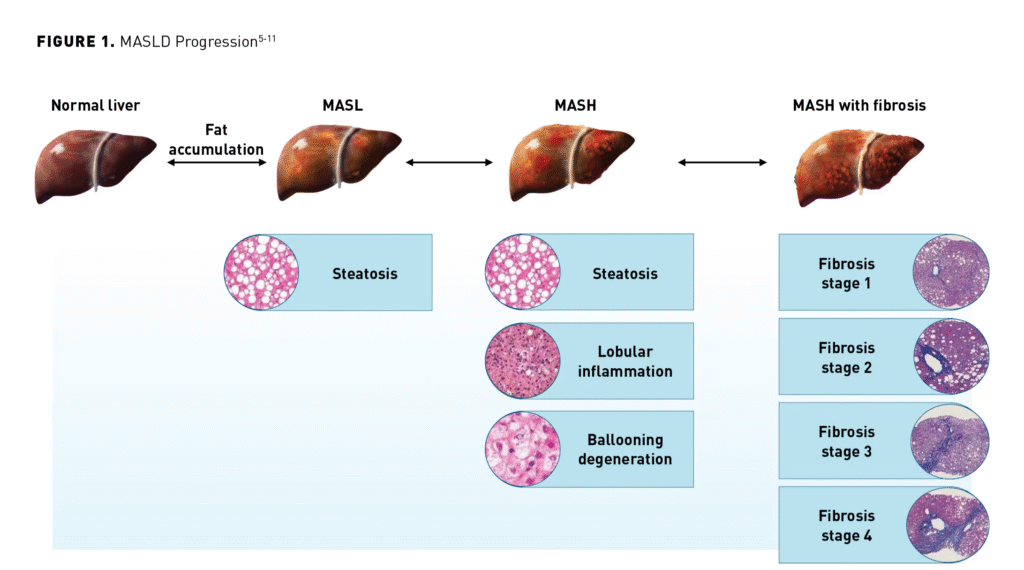
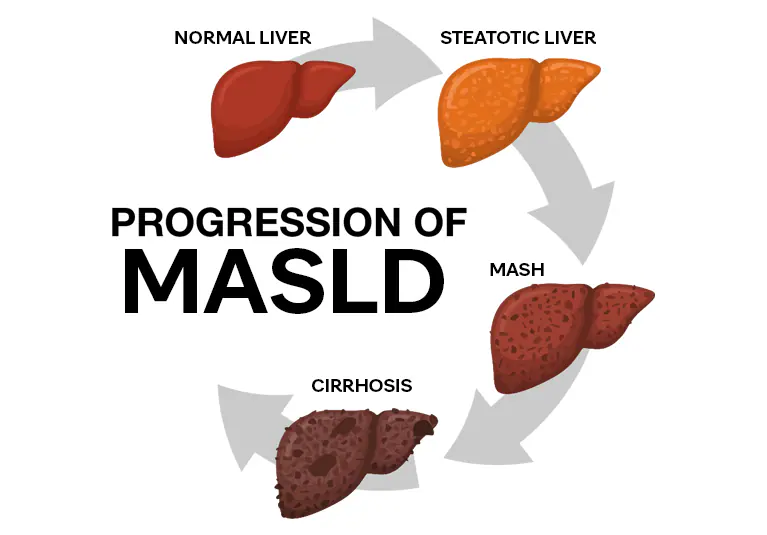
What are the stages of MASLD?
There are several stages of MASLD (also called NAFLD). Having one stage does not mean you will definitely develop the next one. Treating MASLD with a healthy diet, physical activity and weight loss can slow or even reverse liver damage, especially if it is at an earlier stage.
The amount of scarring (fibrosis) in your liver is the main sign of how advanced your MASLD is. Jump to information on tests for scarring.
- Fatty liver (fibrosis stage 0): There is a build-up of fat in your liver but it has not been damaged and there is no scarring. This can be fully reversed.
- MASH or NASH with mild fibrosis (fibrosis stage 0 or 1): There is no or very little scarring. Healthy living can undo the damage and reverse your MASLD.
- MASH or NASH with moderate fibrosis (fibrosis stage 2): Inflammation and damage have caused some scarring. Your liver is probably still working well and the damage can mostly be repaired.
- MASH or NASH with advanced fibrosis (fibrosis stage 3): There is a lot of scarring. At this stage it is very important to stop further damage and scarring so things don’t get worse. And it is still possible to repair some damage.
- Cirrhosis (fibrosis stage 4): There is so much scarring it changes the shape of your liver. Your liver can keep working and even repair some damage at this point. But if too much of it becomes scarred, your liver may not be able to carry out its job properly.
Symptoms and Causes
Symptoms of MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease)
MASLD often develops slowly over many years, and most people don’t notice any symptoms. You may only experience problems if it progresses to MASH (metabolic dysfunction-associated steatohepatitis).
MASH can cause serious liver damage, such as fibrosis (scar tissue) or cirrhosis. When this happens, some people may develop symptoms like:
A dull ache or discomfort in the upper right side of the abdomen (where the liver is located)
Ongoing tiredness or weakness
Loss of appetite
A swollen or bloated belly
Unexplained weight loss
Yellowing of the skin and eyes (jaundice)
👉 Many people with MASLD don’t realize they have it until the disease has advanced, which is why regular health check-ups are important if you have risk factors like obesity, type 2 diabetes, or heart disease.
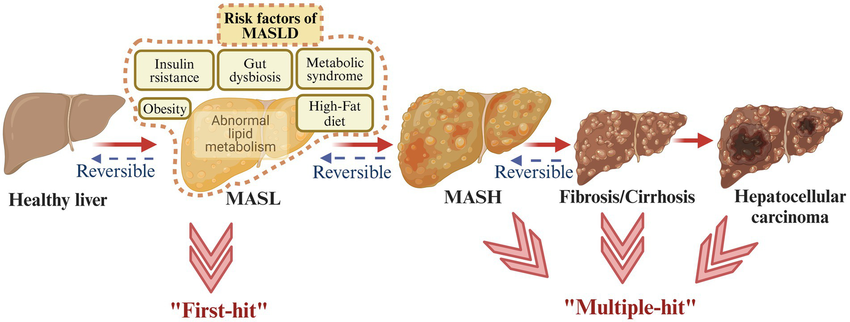
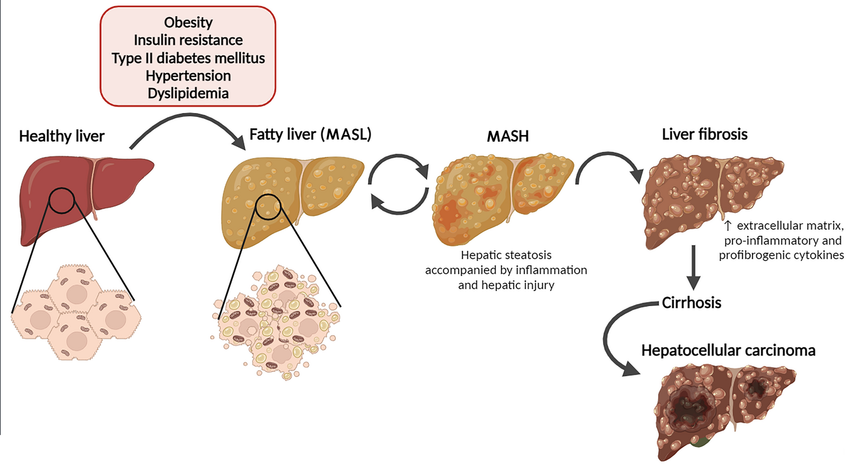
What causes MASLD?
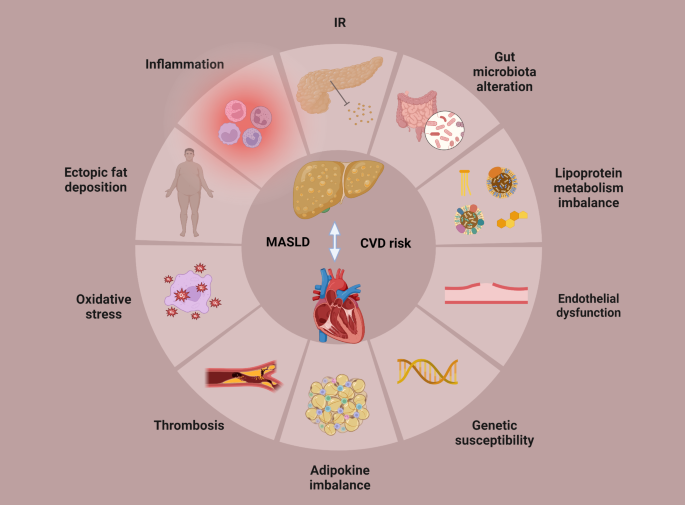
You may develop MASLD if you have metabolic dysfunction. This is a group of conditions that affect your metabolism. Your metabolism changes food into energy. Conditions that may lead to MASLD are:
- Dyslipidemia. This is high levels of lipids. Lipids are fatty or waxy substances that your body makes. Cholesterol is an example of a lipid in your blood.
- Having obesity. Obesity is when your body mass index (BMI) is 30 or higher. People who carry extra weight in their belly have an increased risk of MASLD.
- Insulin resistance. Insulin is a hormone that manages blood glucose (sugar levels). Insulin resistance happens when cells in your muscles, fat and liver don’t respond to insulin as they should.
- Type 2 diabetes. This is a chronic (long-term) condition that happens when you have high blood sugar (hyperglycemia).
Researchers have also found several genetic variations that increase MASLD risk.
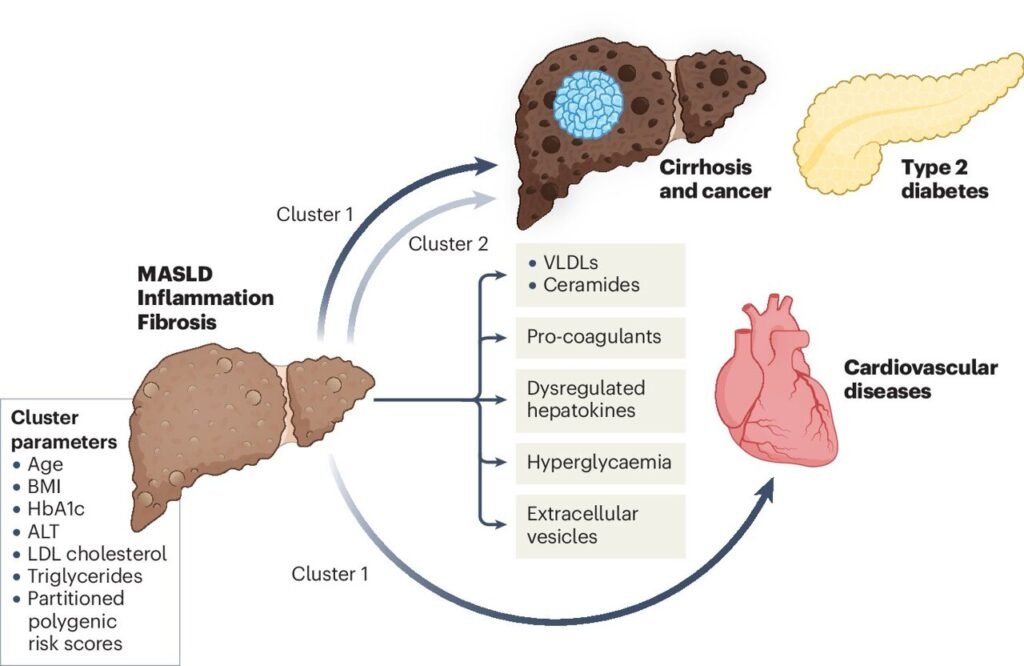
What are the complications of metabolic dysfunction-associated steatotic liver disease?
Some people with MASLD may develop MASH. The condition can lead to more serious forms of MASH, including:
- MASH with liver fibrosis. Fibrosis is bands of scar tissue in your liver. Fibrosis happens when your liver tries to repair and replace damaged cells.
- MASH-related cirrhosis. This is scarring that damages your liver.
- Hepatocellular carcinoma. This is a type of liver cancer that can be caused by MASH.
MASLD may also increase your risk of developing serious conditions like:
- Cancer, including breast cancer and colorectal (colon cancer)
- Cardiovascular disease
- Diabetes in people who don’t already have diabetes
Diagnosis and Tests
How do healthcare providers diagnose MASLD?
Healthcare providers will do certain blood tests and imaging tests (or a liver biopsy).
Blood tests
- A1C. This test measures the average amount of sugar (glucose) in your blood over the past two months.
- Complete blood count (CBC). This test measures the amounts and sizes of your blood cells.
- Comprehensive metabolic panel (CMP). This is a measurement of 14 substances in your blood like proteins and electrolytes.
- Lipid panel. This is a screening test for cardiovascular disease. It measures certain fat molecules in your blood.
- Liver function tests. These blood tests measure substances that your liver produces.
Imaging tests
Your healthcare provider may do imaging tests to look for signs of MASLD in your liver. Tests include:
- FibroScan®. This imaging test estimates the amount of fat and fibrosis in your liver.
- Magnetic resonance elastography and proton density fat fraction (MRE-PDFF). This test measures the percentage of fat and fibrosis in your liver.
Biopsy
Occasionally, your provider may perform a liver biopsy. They may do this if they think something other than MASLD causes your symptoms. They may also do a liver biopsy as a follow-up to imaging tests like FibroScan.
Management and Treatment
Treatment for MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease)
The main goal of treating MASLD is to reduce fat in the liver and improve overall health. Treatment usually begins with weight loss and managing related conditions like diabetes, high cholesterol, and high blood pressure.
Weight loss: Even a small amount of weight loss helps. Losing 3–5% of your body weight can improve liver health, and losing 10% or more can make an even bigger difference.
Healthy eating: Your provider may suggest following meal plans such as the Mediterranean diet or the DASH diet, which focus on fresh fruits, vegetables, whole grains, lean proteins, and healthy fats.
Regular activity: Doing moderate exercise for at least 30 minutes, three times a week supports weight loss and improves liver function.
Managing other conditions: Treating diabetes, high cholesterol, and high blood pressure helps slow or prevent liver damage.
👉 Lifestyle changes are the most effective treatment right now, but researchers are studying new medicines that may help in the future.